TC
-
Ground-glass opacity
-
Multiple lobes
-
Subpleural or peripheral distribution (center is usually preserved)
-
Septal thickening
-
Bronchial thickening
-
Pulmonary consolidations / “crazy paving” pattern (advanced di)
-
Predominantly peripheral, basal and generally bilateral
-
No nodules, no pleural effusion, no cavitation
- Ground-glass opacity and peripheral distribution (subpleural)
Ground-glass opacity is a descriptive term referring to an area of increased attenuation in the lung with preserved bronchial and vascular markings.
-
Multiple lobes
- Septal and bronchial thickening
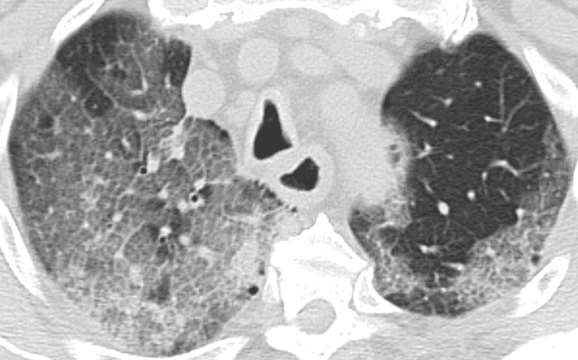
- Crazy paving
The “crazy-paving” pattern is a common finding at thin-section computed tomography (CT) of the lungs. It consists of scattered or diffuse ground-glass opacity with superimposed interlobular septal thickening and intralobular lines that give the illusion of polyhedral shapes that resemble paving stones.
- ASYMPTOMATIC STAGE
Ground-glass opacity areas, frequently unilateral and multifocal. - FIRST WEEK AFTER SYMPTOM ONSET
Pulmonary lesions become bilateral, more extensive, diffuse with multiple segment affectation. The predominant pattern is peripheral ground-glass opacity, with ill-defined margins, but it can also be central. In some cases, "crazy-paving" in present. Some cases also present thickening of the adjacent pleura. Less common findings are pleural effusion and lymphadenopathies. - SECOND WEEK AFTER SYMPTOM ONSET
Ground-glass opacity pattern decreases and consolidation areas appear (usually presenting organizing-pneumonia features). - EVOLUTION TO ARDS
Radiographic improvements are related to favourable outcomes in most patients. Some patients undergo complications and evolve to an ARDS clinical presentation.
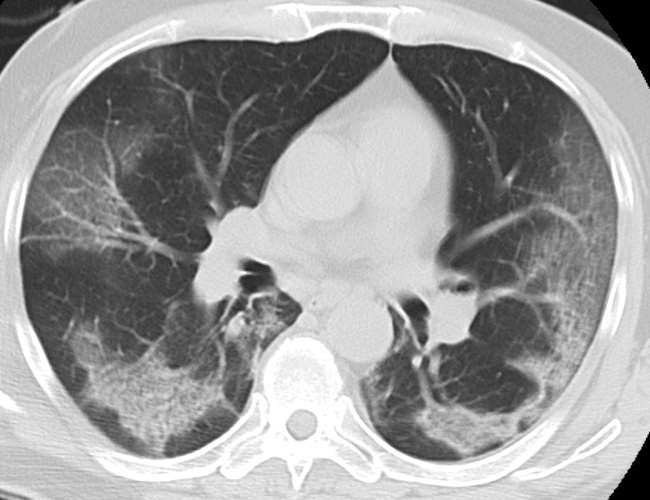
Clinical case 1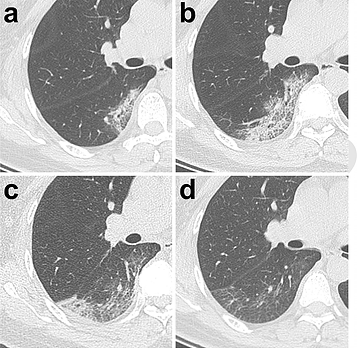
47-year-old-woman with 3-day-long-fever (38,8ºC)
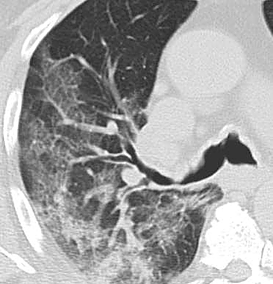
- Day 3: ground-glass opacities located in a small subpleural region and partial consolidation in the inferior right lobe.
- Day 7: the region where ground-glass opacities were located expands. Septal thickening (both interlobular and intralobular, also known as "crazy-paving") appears. Partial consolidation is also present.
-
Day 11: ground-glass opacity pattern partially resolves. A new area of subpleural consolidation appears.
-
Day 20: ground-glass opacity pattern resolution continues. Prenchymal lines are present.
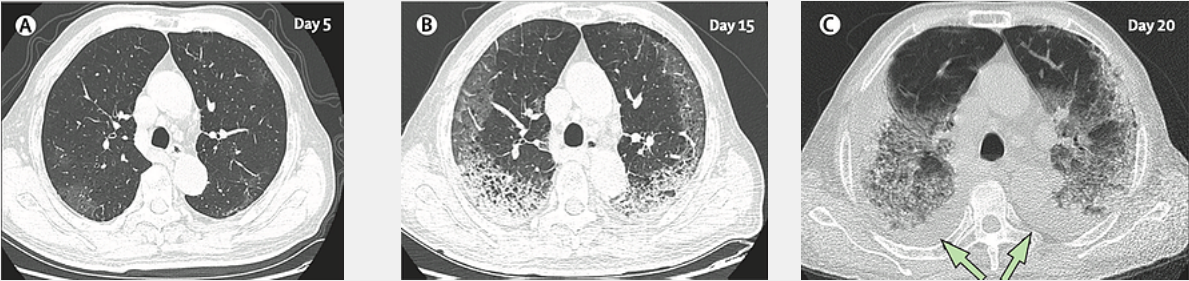
Clinical case 2
77-year-old male
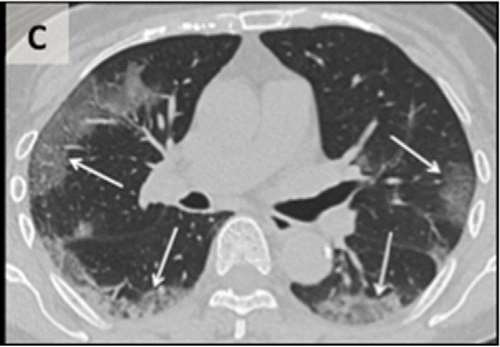
- Day 5 after symptom onset.
Patchy ground-glass opacities affecting the bilateral, subpleural lung parenchyma.
-
Day 15 after symptom onset.
Subpleural crescent-shaped ground-glass opacities in both lungs, as well as posterior reticular opacities and subpleural crescend-shaped consolidations. -
Day 20 after symptom onset.
Expansion of bilateral pulmonary lesions, with enlargement and denser pulmonary consolidations and bilateral pleural effusions (arrows). The patient died 10 days after the final scan. The patient died 10 days after this CT.
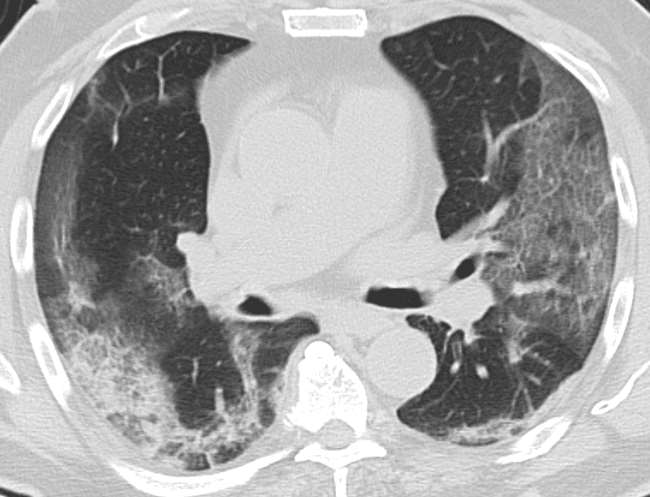
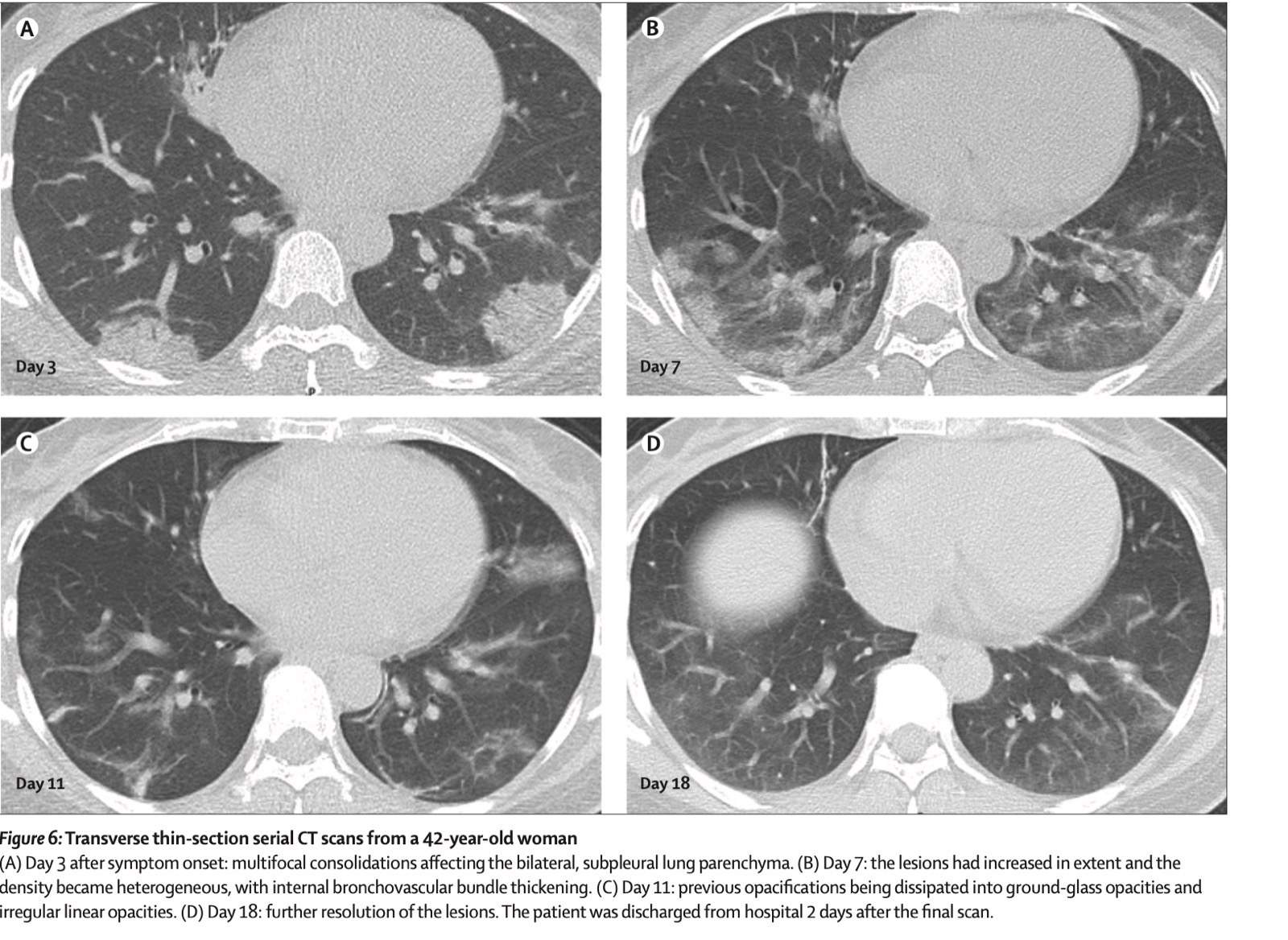
Clinical case 3
42-year-old female
- Day 3 after symptom onset: multifocal consolidations affecting the bilateral, subpleural lung parenchyma.
- Day 7: the lesions had increased in extent, and the density became heterogeneous, with internal bronchovascular bundle thickening.
-
Day 11: previous opacifications being dissipated into ground-glass opacities and irregular linear opacities.
-
Day 18: further resolution of the lesions. The patient was discharged from hospital 2 days after the final scan.
Other rare findings that might be found
-
Pleural thickening
-
Bronchiectasis
-
Pleural effusion
-
Lymphadenopathies
There are radiologic patterns that can appear exceptionally in these patients patients and they are indicative of an alternative diagnosis:
-
Lobar localized lesion
-
Cavitation
-
"Tree in bud" sign
-
Calcification
-
Pneumothorax
-
Mass
-
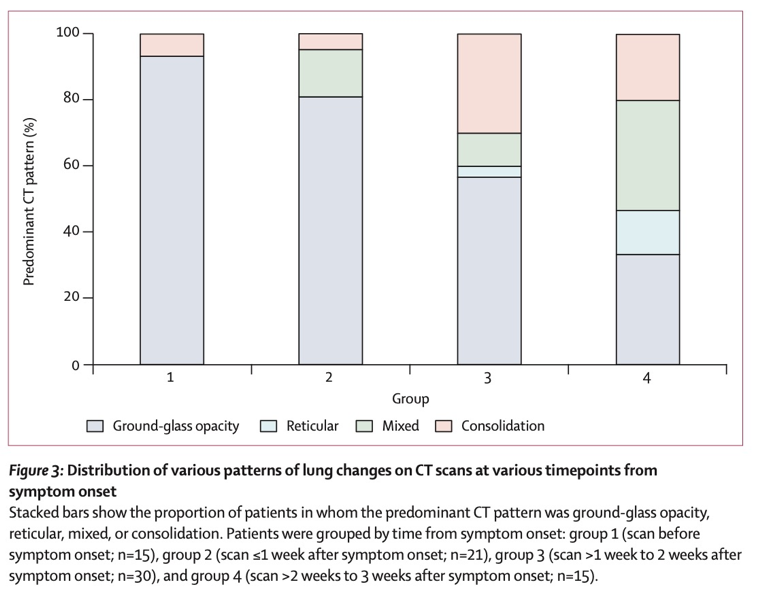
In the asymptomatic stage, the most common finding is ground-glass opacity (present in 90% of patients).
-
During the first week the findings remain the same. However, in some cases signs of consolidation appear.
-
During the second week, after the symptom onset, the number of cases with ground-glass opacities decrease whereas sign of consolidation or the coexistence of both patterns (ground-glass opacity + consolidation) increase.
-
During the third week, most patients present a mixed pattern.
- Ai, T., Yang, Z., Hou, H., Zhan, C., Chen, C., Lv, W., … Xia, L. (2020). Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology, 200642. https://doi.org/10.1148/radiol.2020200642
- Bernheim, A., Mei, X., Huang, M., Yang, Y., Fayad, Z. A., Zhang, N., … Chung, M. (2020). Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology, 200463. https://doi.org/10.1148/radiol.2020200463
-
Casais, M. C. A., Crujeiras, C. V., Ariza, M. V. T., & Gutierrez, B. (2012). Crazy paving. ¿Un patrón que ayuda o confunde? Seram (Vol. Poster S-1). https://doi.org/10.1594/seram2014/S-1113
-
Franquet, T. (2012). Diagnóstico por Imagen de las Enfermedades Pulmonares Difusas: Signos y patrones diagnósticos básicos. Medicina Respiratoria, 5(3), 49–67.
-
Han, R., Huang, L., Jiang, H., Dong, J., Peng, H., & Zhang, D. (2020). Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) Pneumonia. American Journal of Roentgenology, 1–6. https://doi.org/10.2214/AJR.20.22961
-
Holshue, M. L., DeBolt, C., Lindquist, S., Lofy, K. H., Wiesman, J., Bruce, H., … Pillai, S. K. (2020). First Case of 2019 Novel Coronavirus in the United States. New England Journal of Medicine, 382(10), 929–936. https://doi.org/10.1056/NEJMoa2001191
-
Moy, L., & Bluemke, D. (2020). The Radiology Scientific Expert Panel. Radiology, 204005. https://doi.org/10.1148/radiol.2020204005
-
Pan, F., Ye, T., Sun, P., Gui, S., Liang, B., Li, L., … Zheng, C. (2020). Time Course of Lung Changes On Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19) Pneumonia. Radiology, 200370. https://doi.org/10.1148/radiol.2020200370
-
Rozas Gómez, I., Garcia Hernando, T. M., López-Vidaur, I., Armendariz Blanco, L. I., Olmedilla Arregui, P., & Quintana Checa, V. (2014). Crazy paving. ¿Un patrón que ayuda o confunde? SERAM, S-1319. http://dx.doi.org/10.1594/seram2014/S-1319
-
Salehi, S., Abedi, A., Balakrishnan, S., & Gholamrezanezhad, A. (2020). Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. American Journal of Roentgenology, 1–7. https://doi.org/10.2214/ajr.20.23034
-
Shi, H., Han, X., Jiang, N., Cao, Y., Alwalid, O., Gu, J., … Zheng, C. (2020). Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. The Lancet. Infectious Diseases, 20(4), 425–434. https://doi.org/10.1016/S1473-3099(20)30086-4
-
Smithuis, R., Van Delden, O., & Schaefer-Prokop, C. (n.d.). Lung - HRCT Basic Interpretation. Retrieved from https://radiologyassistant.nl/chest/lung-hrct-basic-interpretation
-
Società Italiana di Radiologia Medica e Interventistica. (n.d.). COVID-19 DATABASE. Retrieved from https://www.sirm.org/category/senza-categoria/covid-19/
-
Thoracic Imaging in COVID-19 Infection. Guidance for the Reporting Radiologist British Society of Thoracic Imaging. 13/03/2020: https://www.bsti.org.uk/media/resources/files/BSTI_COVID-19_Radiology_Guidance_v1_13.03.20_9kzNSRs.pdf